WATCH-Symposium
Datum 20.01.-21.01.2026
Veranstaltungsort: CBBM, Seminarraum Levi-Montalcini
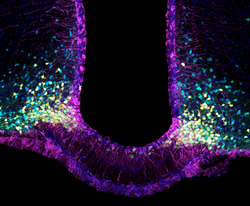
WATCH (Well-Aging and the Tanycytic Control of Health) ist ein Synergy Grant des Europäischen Forschungsrats (ERC), der 2018 gemeinsam an Vincent Prevot (INSERM, Frankreich), Markus Schwaninger (Universität Lübeck, Deutschland) und Ruben Nogueiras (Universität Santiago de Compostela, Spanien) vergeben wurde. Das Verständnis, wie das Gehirn Körperfunktionen reguliert, ist entscheidend für die Bekämpfung von Stoffwechselstörungen und neurodegenerativen Erkrankungen. Das Projekt erforscht die molekularen Mechanismen, die diesem Prozess zugrunde liegen, und konzentriert sich dabei auf die neuroendokrinen und metabolischen Funktionen der Tanyzyten im Hypothalamus. In den letzten sieben Jahren hat die WATCH-Gruppe bedeutende Entdeckungen gemacht. Auf dem Symposium, das am 20. und 21. Januar 2026 in Lübeck stattfindet, werden die Partner die neuesten Erkenntnisse und Perspektiven diskutieren, die aus dem gemeinsamen Projekt entstanden sind.
Weitere Informationen zum ERC-WATCH-Projekt: Home - WATCH
Für weitere Informationen zum Programm der Veranstaltung und zur Anmeldung wenden Sie sich bitte an Aurelie Batchadji unter aurelie.batchadji(at)uni-luebeck(dot)de.
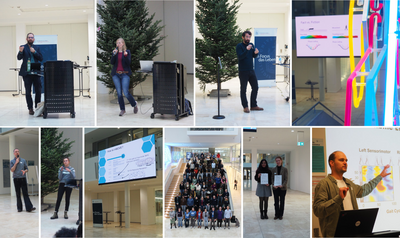
Successful hosting of I-MOVE2025
From December 4-6, 2025, I-MOVE 2025 was hosted on an interdisciplinary basis by the Institute of Psychology, the Institute of Medical Psychology, and the Department of Neurology on the CBBM premises.
The necessity and importance of the conference topic, the integration of movement information into neuroscientific research, was highlighted in the presentations by keynote speakers Freek van Ede (Institute for Brain and Behavior, Vrije Universiteit Amsterdam), Marlene Meyer (Donders Institute for Brain, Cognition, and Behaviour, Radboud University, The Netherlands), and Giacomo Novembre (Neuroscience of Perception and Action Lab, Italian Institute of Technology, Rome) for different neurocognitive disciplines. The demonstrations on handling multimodal data (Julius Welzel, Kiel University) and online synchronization of multimodal data acquisition (Melanie Klapprott and Martin Bleicher, University of Oldenburg) were given as hands-on sessions. The Junior Poster Award went to Vaishali Vinod (Kiel University, “Preprocessing on the Move: An Overview of Preprocessing Pipelines in Gait-related Mobile EEG”) and Annika Werwach (Max Planck Institute for Human Development, Berlin, “Memories in motion: Tracking memory development in freely moving toddlers using mobile EEG”). We would like to thank all participants for making I-MOVE 2025 a success. Special thanks go to our student team for their tireless efforts.